
When China reported the emergence of a mysterious new virus at the end of December 2019, the news was a red flag for scientists and physicians who study infectious diseases. The notion that it could be the beginning of a pandemic was not farfetched. Pandemics such as the Black Plague in the Middle Ages and the Spanish Flu in 1918 have ravaged populations around the world periodically throughout history. Another one was inevitable, but when it might strike was impossible to predict, and it was one of the public health community’s greatest fears. In an era of easy communication and sophisticated research, however, it was reasonable to think that should a disease with the potential to become a pandemic appear, it would be possible to take measures to mitigate it. Nonetheless, once the virus gained a foothold, it spread rapidly, and within weeks, it reached Europe and the United States and infected every continent except Antarctica.
Dean Winslow, M.D. a professor of medicine in the Division of Diseases and Geographic Medicine at the Stanford University School of Medicine, first read reports about a new coronavirus in January, when he and his wife were working as doctors in Antarctica. He recognized the threat, but didn’t foresee its rapid expansion. “I personally didn’t think the disease would become a pandemic this quickly,” he says. When they returned to California in February, however, he faced an alarming reality. The virus, named SARS-CoV-2, had crossed oceans and borders, causing a respiratory disease called COVID-19. It was on its way to becoming a full-fledged pandemic, putting the onus on medical researchers to find effective treatments and a vaccine as quickly as they could.
Origin and infection
Human coronaviruses are invisible without a microscope, but they are quite common. The Centers for Disease Control and Prevention (CDC) reports that they were identified first in the 1960s, and seven different types, including the common cold, can infect humans. SARS is an acronym for severe acute respiratory syndrome. In 2003, the beta coronavirus SARS-CoV caused an epidemic infecting 8,000 people in 26 countries. SARS-CoV-2 is a novel—or new—coronavirus that is related to the earlier strain, and although nobody knows exactly where it originated, Winslow believes the most likely source is bats.
Winslow, who is familiar with coronaviruses and also has experience studying Human Immunodeficiency Virus (HIV), explains that SARS-CoV-2 is a zoonotic virus—one that begins in an animal and jumps to humans. Many other coronaviruses originated in bats. “Bats are the natural reservoir. Humans are accidentally infected,” he explains. (Similarly, the host for influenza is birds, and all flu is “bird flu.”) Several of the early cases in China were traced to the 12-acre Huanan Seafood Market—or wet market—in Wuhan, a city of several million people. The market houses stalls where vendors sell live fish, wild animals and freshly-butchered meat, and it’s an environment where viruses from different species can circulate and spread. Winslow suspects SARS-CoV-2 might have had an intermediate host, perhaps a pangolin, which is a small, scale-covered mammal. Pangolins are a protected species, but a large illegal trade flourishes, as its scales are used in traditional Chinese medicine and folk remedies. One may have ended up at the market and transmitted the virus from bats to humans.

Once SARS-CoV-2 makes the leap to humans, the transmission is remarkably efficient. It’s an RNA virus that infects humans when they inhale air droplets originating from a nearby person who is shedding the virus. The spikes that give a coronavirus cell its characteristic appearance (corona is Latin for crown), bind it to a healthy cell in the host’s airway, and it injects an RNA strand into the cell. The RNA then produces a protein that causes the viral cell to replicate, overwhelming the host cell. “It’s a slick mechanism,” says Winslow, explaining that as the virus is released, it uses cytoplasmic structures to assemble, and it destroys the host cell.
The result is COVID-19, a disease that attacks the respiratory system and damages other organs. And because symptoms can vary dramatically from one individual to another, it has an unpredictable course. Some people show either minimal symptoms or none at all, while it can be deadly for others. “What makes this particular pathogen unique is that it causes a very severe level of fatal disease in a large number of people,” Winslow says. He points out that people with comorbidities such as diabetes, heart disease and lung disease are particularly vulnerable, thus accounting for the high mortality rate. Although likely, it’s uncertain if those who have recovered from COVID-19 have developed immunity, so whether reinfection can occur has yet to be determined. “Antibodies to SARS-CoV-2 are definitely being produced, but we don’t know for sure if they are protective, nor the duration of protection,” says Winslow. He reports that in a study of four experimentally-infected monkeys, the animals produced neutralizing antibody responses to the viruses, protecting the monkeys from re-infection with SARS-CoV-2 when they were re-challenged with the virus 28 days after initial infection. However, we don’t know how long this protection lasts in monkeys or in humans.
The World Health Organization (WHO) declared COVID-19 a pandemic on March 11, and taking action to combat it became a worldwide priority. SARS-CoV-2 is highly contagious, and the first step should have been putting effective measures into place to contain the virus, but that required large-scale testing to give a big picture of the disease, and in the U.S., testing kits were in short supply. “For a variety of reasons, the rollout of diagnostics was rather slow,” says Winslow. The lack of widespread testing limited the ability of state and local health departments to put effective control measures into effect quickly, he adds, because they didn’t have enough information. For example, testing helps to determine the R0 (pronounced R naught) value, a mathematical indicator of the number of people one individual can infect. It’s useful in predicting the rate of infection when everyone is vulnerable to a disease, which is the case with COVID-19 because nobody has had the disease before, and a vaccine isn’t available. “It’s important to effectively deploy forces guided by good intelligence data,” says Winslow, because it shows how to use resources best and determines what kinds of preventive measures are reasonable.
Because SARS-CoV-2 is airborne and easily spread, measures such as diligent handwashing and avoiding touching one’s face are important, but they aren’t sufficient to stop the virus from spreading. As a result, on March 16, six San Francisco Bay Area counties—San Francisco, Santa Clara, San Mateo, Marin, Contra Costa and Alameda—ordered their residents to shelter in place beginning at 12:01 a.m. the following day. Napa and Sonoma counties quickly followed, and then on March 20, California Governor Gavin Newsom extended the shelter-in-place order to the entire state. Much of normal everyday life came to a standstill, as millions of people adjusted to spending most of their time at home, going out only for essential needs such as shopping for food or getting prescriptions filled. When they did go out, they had to maintain social distancing and stay at least 6 feet away from others, and the CDC recommended wearing masks so that asymptomatic individuals wouldn’t unknowingly infect others. “It’s unprecedented in the effect it’s had on the world,” says Winslow, observing that it’s devastating from a business and economic standpoint as well as from a health perspective. He commends Sara Cody, M.D., health officer for Santa Clara County, for spearheading a rapid response with a regional approach that’s proven to be effective.
Strategies
For county health departments, the initial challenge was finding people who’d been infected. “In any infectious disease, having accurate diagnostic testing is the first step. It’s the same as measles or meningitis,” says Lisa Santora, M.D., M.P.H., deputy public health officer for Marin County. She explains that when a person tests positive, the results are reported to the local health department, and the patient has to follow isolation orders. The information also goes into a dashboard or tracking system, and a public health nurse launches an investigation to trace all the infected individual’s recent contacts. If they’re at risk, they’re required to go into quarantine for a prescribed period of time. The goal is to slow down transmission, thereby lessening the upward trajectory of infection and flatting the statistical curve.
A substantial number of people are asymptomatic, however, and in the absence of signs they could be infected, they don’t get tested. “For every positive test, there are probably 99 undiagnosed cases,” says Santora, who estimates that in April, as Marin County approached its projected peak infection, between 5,000 and 10,000 people in Marin County had COVID-19 but didn’t know it. One concern was that some of them might be staff at health-care facilities or nursing homes. “As a health-care worker, before you enter a hospital, you have to prove that you’re immune to measles,” she says, but that’s not yet possible for SARS-CoV-2. “We’ve had to prioritize testing for the most vulnerable,” she explains. “Until we know more about immunity, we would not recommend universal testing for everybody. We’re still very much in a learning-research stage in our country and globally.”
Sonoma County also put testing and tracking into place, and by mid-April, Sundari Mase, M.D., the county’s health officer, was cautiously optimistic that the measures were having the desired effect. The initial cases were either people who had traveled or become infected in the community, but later reports showed that community transmission was minimal. She suspects the shelter-in-place order is responsible for the low numbers. She cautions, however, that it would take just one case for the entire picture to completely change. “Without any mitigating measures, we could have seen up to 10,000 bed needs at the peak of infection,” she says. “The shelter-in-place has been much more successful than expected. We are flattening the curve, but it’s something we can only do with full involvement.”

Meanwhile, the biggest challenge is fear, since so much is unknown. “I empathize with our community facing a once-in-a-century event,” says Santora, observing that people weren’t prepared for such a situation. However, she adds, “We have very defined strategies. We have a tremendous team. Our communicable disease team has been working on this since January.” She reports that it was difficult for health officials to take such a drastic measure as shelter-in-place. “It was a fraught decision because we knew the economic impact this would have on the most vulnerable residents of our community,” she says. In addition, she adds, the social disruption further isolates the homeless, low-income earners and at-risk people who are already alone. By mid-April, though, the results were starting to show. “The decision to take aggressive measures is affirmed by data that shows we are flattening the curve,” she says. It is, however, important to be vigilant because loosening the restrictions too soon could result in spikes and a surge, which is like a rebound effect. “We know how hard and challenging it is for some to shelter in place. Restricting activities is not normal and is not what we desire,” she says. “It takes all of us working together. Staying home is literally saving lives.”
Research
The human immune system has two mechanisms for preventing infection. The innate immune system is the first level, and it consists of the skin and mucous membranes. If it is unable to prevent germs from entering the body, the adaptive immune system takes over. Its defense cells and proteins create antibodies to fight the intruder from the inside. Because SARS-CoV-2 gets past the initial defenses, the adaptive immune system is the primary focus of current research, which includes seeking treatments, a vaccine and an antibody test.
The innate immune system becomes dysfunctional in older adults, resulting in chronic inflammation, and as it becomes less effective, the adaptive immune system can play a larger role in fighting infections. Therefore, studies on aging that focus on both the innate and adaptive immune systems also apply to research into SARS-CoV-2, and some of the work at the Buck Institute for Research on Aging in Novato is valuable in the search for ways to treat and prevent COVID-19, given that older adults are more at risk of complications from the disease. “The history of the Buck in doing research on aging is incredibly important,” said Eric Verdin, M.D., president and chief executive officer, in an online presentation in April. Verdin’s lab is part of an international collaboration that is examining and testing drugs that show promise in fighting the virus.
Verdin reported that Nevan Krogan, Ph.D., a biologist at the Gladstone Institutes at the University of California San Francisco, as well as an adjunct faculty member at the Buck, studied the genes of SARS-CoV-2 and mapped human proteins that interact with it. Krogan then led an international collaboration that included Gladstone researcher Melanie Ott, who is also and adjunct faculty at the Buck. Scientists identified close to 70 existing drugs and experimental compounds that showed promise against COVID-19. Some of the proteins and drugs identified in the research impact the aging process.
Among the drugs that emerged in the studies are rapamycin, which is an immune suppressant; metformin, a medication for treating diabetes; and remdesivir, a drug that was developed to fight Ebola during the epidemic in Africa in 2014 but wasn’t effective. Remdesivir shows promise because it works to inhibit the coronavirus protein that allows the virus to replicate. Hydroxychloroquine, which is used to treat malaria, rheumatoid arthritis and lupus, is better known, but while it works in the lab, it needs more study to prove that it’s effective and safe against COVID-19. Verdin advises people already taking the drugs under study to continue taking them, but not to change the dose. The effects aren’t linear, he says, adding, “Taking more doesn’t mean you get a better effect.” He also reports that one person taking hydroxychloroquine for another condition increased the dose and subsequently developed cardiac arrhythmia and died. “These drugs carry significant risk of complications,” he says. “It’s not the time to experiment with anything.” He explains it’s up to scientists to understand precisely how the virus works and how drugs interfere with the virus’s process. And that, he says, is going to take time.
The same is true of a vaccine because the FDA requires clinical trials to determine its efficacy and safety. Verdin explains that in the classical method of developing a vaccine, scientists take a virus, make it multiply in a lab setting and then disable it. Injecting the resulting vaccine into people then induces immunity. “It’s very likely we’ll be able to produce a vaccine,” he says. However, it’s an exacting and time-consuming process with an unknown timeframe. Antibody or serological tests are also important because if it’s established that people develop immunity after being infected, it would be a useful tool for determining herd immunity. “The more people are immune, the fewer the virus can infect,” says Verdin.
What the future holds is uncertain. Smallpox has been eradicated, and only a few cases of polio remain, but they are viruses with a human host. With SARS-CoV-2, the challenge is developing a vaccine for a virus that originates in an animal. “It would be difficult because small mammals are the natural host,” Winslow says, explaining that makes it likely that the virus will return with variations, as does the flu.
Looking ahead
To deal with a future pandemic, Verdin emphasizes the need for improvements in the public health system, observing that for the last 40 years, there has been a disinvestment in public health. “The science of epidemiology hasn’t had enough attention,” he says, and although it would be costly, it would pale in comparison to the price we’re paying now. “Hopefully, we’ll move into supporting a stronger public health system,” he says, predicting that this pandemic won’t be the last. “Potential pathogens could be worse,” he says, explaining that they’re lurking in animals, waiting to jump to humans. “We have to mitigate what happens when a jump occurs because we can’t prevent it.”
Undeniably, some things could have been done differently and better. Winslow points out that the CDC usually has staff stationed in China, but as a result of geopolitical issues that led to a poor relationship between the U.S. and China, it didn’t have representation as usual in the crucial early days of infection. “That could have been very helpful,” he says, as would a national shelter-in-place.
The scientific community, on the other hand, came together in a way that was extraordinary. Verdin observes that scientists put aside their usual competition to work collaboratively on COVID-19, sharing ideas that put research on a productive path. “It’s a new way to do science,” he says. “I find it incredibly refreshing.”
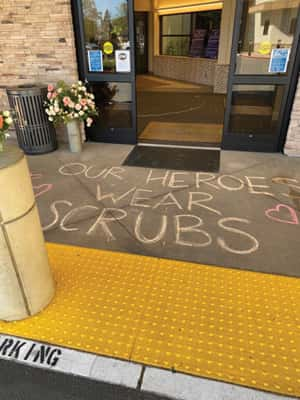
The dedication of health-care workers and staff is also admirable. “They provide the highest level of care,” says Santora, and even though they’re putting themselves at risk and worry about taking the virus home to their families, they continue working. Sometimes, adversity brings out the best in people, and their example gives us hope, as we look ahead to rebuilding and creating a better future.
By Judith M. Wilson